Scientific Overview in Historical Context
 The World Health Organisation provides a comprehensive and accurate description of the disease. *1
The World Health Organisation provides a comprehensive and accurate description of the disease. *1
Even though leprosy has been present throughout the world earlier than recorded history, leprosy is a mysterious disease about which very little has been known until recently. From a historical point of view what we now know as leprosy was called many different names in many different locales and this was further complicated because different people exhibited many different symptoms. It took some time before medical people decided that what was being observed was a single disease entity.
In 1875, Ferdinand Hebra and Moritz Kaposi‘s On the Diseases of the Skin Including the Exanthemata lists the many names which identified the disease in various countries throughout the world.*1 They also noted the variety of names that described symptoms of the disease. There was added confusion encountered in Adams that stretched back to the Biblical translation of the Hebrew zaraath as lepra:
When, in the course of the 14th century, the writings of the Greek and Roman authors were again brought to light, and began to be studied in the original, it became evident that the nomenclature of lepra was involved in great confusion. The dangerous constitutional disease under discussion was called Djudzam by the Arabians, an expression which is still in vogue among the Persians, and was translated by the word “Lepra.” It was now discovered that the lepra of the Hippocrates and the Greeks was a simple scaly disease and that whilst they had undoubtedly described the disease called Djudzam by the Arabians (of which the translation is lepra), they had given it the name “Elephantiasis.” (125)
Hebra and Kaposi had to make a distinction between “Lepra Arabum-Elephantiasis Graecorum”; “Elephantiasis Arabum”; and “Lepra Graecorum”, terms which had been used indiscriminately to denote different diseases occurring in the same region or in the same individual, or used in place of some other skin afflictions including syphilis. They remarked that almost any “rare, disfiguring, incurable, or exotic diseases” may have been diagnosed as leprosy, contributing to the confusion over in what precisely the disease might actually consist. As a result of persisting terminological and diagnostic confusions, regional comparisons and thus clear identification of the disease became even more difficult:
Owing to the conflicting views, everyone was quite at a loss to determine whether, and in what manner, certain diseases, supposed to be endemic, such as the Radesyge of Norway, the Morbus Dithmarscicus, the Sibbens of Scotland, the Falcadina of Istria, were connected with lepra. (127)
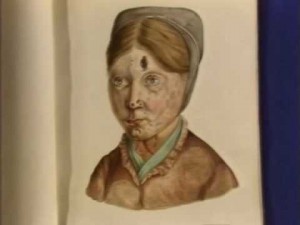
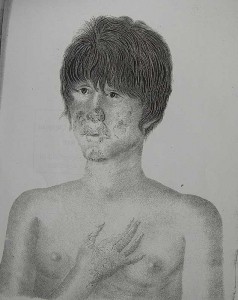
One of Losting’s famous portraits of a woman with leprosy in St Jørgen’s Hospital, Bergen, Norway
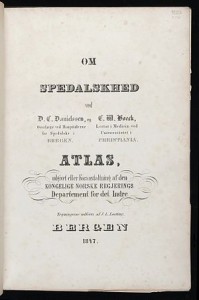
Hebra and Kaposi cite Danielssen and Boëck as having supplied the first clear description of the pathology of the disease. They then state emphatically that this much is now known: “that wherever lepra exists, at the present time, it always presents the same characters, and that the lepra of all countries is identical” (131). In addition, they determine that differences in symptoms in various localities are not significant and do not represent different varieties of the disease. Therefore, “in consequence of this discovery, all the names hitherto applied to the disease which are derived from its geographical position … must be given up, and one designation, founded on the history of the disease, and which may be understood by the physicians of all countries, must be substituted for them, once for all.” (131) They pronounce Lepra to be the name which they will use in future.
You Tube: On Leprosy (based on Danielssen and Boëck’s Atlas)
 There were differences in how the disease presented itself in people living in the same area or in groups in different areas: “Cases of it differ widely in regard to form, localisation, the organs of the tissues affected, in the order, combination, duration, and intensity of the symptoms, and in the extent to which the system is affected” (135). Different individuals were affected to different degrees over different time spans: “the time of appearance, the duration, or the severity of the symptoms, may give rise to variation, and many of them may remain of secondary importance, or be altogether absent” (135). In fact, there is a problem in identifying forms of lepra because “they often pass imperceptibly into one another, or combine together, and may all be met with at once on the same individual” (135). As a result, depending on who has seen what, at what particular point in the course of the disease, certain features of the disease could be emphasised over others.
There were differences in how the disease presented itself in people living in the same area or in groups in different areas: “Cases of it differ widely in regard to form, localisation, the organs of the tissues affected, in the order, combination, duration, and intensity of the symptoms, and in the extent to which the system is affected” (135). Different individuals were affected to different degrees over different time spans: “the time of appearance, the duration, or the severity of the symptoms, may give rise to variation, and many of them may remain of secondary importance, or be altogether absent” (135). In fact, there is a problem in identifying forms of lepra because “they often pass imperceptibly into one another, or combine together, and may all be met with at once on the same individual” (135). As a result, depending on who has seen what, at what particular point in the course of the disease, certain features of the disease could be emphasised over others.
Nonetheless, they provide a detailed general symptomatology as well as descriptions of lepra tuberosa, lepra maculosa, and lepra anaesthetica, which they differentiate from syphilis, lupus, sarcoma pigmentodes, and vitiligo. Finally, they conclude their discussion of the disease with a call to end the confusion: “Let us hope that the continued co-operation of many able investigators, such as hitherto have been at work in this direction, under the stimulus of science, governments, and philanthropy, will succeed in clearing up the mystery” (193). *3
Gerhard Henrik Armauer Hansen
When Gerhard Henrik Armauer Hansen described leprosy In Leprosy: in its Clinical and Pathological Aspects, he examined a section of fresh nodules under the microscope and observed small straight rods in the fluid of the preparation. These were the lepra bacilli that he first discovered in 1871 (Hansen et al., 1895, p. 31). In a fresh preparation, they could be observed to be moving actively. He described them in larger or smaller clumps of a brownish colour that were very granular. They were in the cells and in all the other organs affected with leprosy. He suggested that they may very well serve as a diagnostic indication for leprous affections because, in his experience, they were always present, except in very young nodules.
He remarked that the bacilli must increase very, very slowly and that they probably produced a toxin in very small quantities which “causes no particular injury to the organism, since patients, in spite of numerous nodules with millions or milliards of bacilli, may remain in pretty good health for years.” (Hansen et al., p. 40) He also identified bacilli that broke down into granules as ones that had degenerated. In his numerous attempts to cultivate the bacilli, he had managed only to attain granules. He wrote that “As the bacilli at first multiply in the cells, and the breaking down appears most definitely and freely when the cells are crammed full of bacilli, it is equally possible that it is the result of diminished nutrition, and as they break down more rapidly in the internal organs, it is also possible, indeed probable, that the higher temperature in these organs favours disintegration. As we have unfortunately not been able to cultivate the bacilli, it is at present impossible to form a conclusion. At all events, we regard the transformation into granules as a degeneration, and believe that the bacilli this altered are dead.” (Hansen et al., 1895, pp. 42-3.)
He also remarked that: “As we do not know the manner and method of the primary infection of the organ, we must devote our attention to the search for discoveries like those described above, and to the localisation of the bacilli in general, in order to form an idea of the method of action of the bacilli.” (Hansen et al., 1895, p. 39) *4

Charles Shepard
It would be more than one hundred years before the bacilli could be cultivated under laboratory conditions. In 1960, Charles Shepard submitted two important papers: to the American Journal of Hygiene (later to be renamed the American Journal of Epidemiology) and to the Journal of Experimental Medicine. The first was entitled “Acid-Fast Bacilli in Nasal Excretions in Leprosy and Results of Inoculation of Mice” and the second was “The Experimental Disease that Follows the Injection of Human Leprosy Bacilli into Foot-Pads of Mice”. In these papers he recounted the experimental process that led to the multiplication of M leprae in laboratory conditions. Taking his cue from the Australian scientist, Frank Fenner, who had cultivated Mycobacterium balnei (later renamed M. marinum) and M ulcerans in the mouse foot pad, Shepard suspected that he could do the same with M leprae. He wrote that this “success in the mouse foot-pad with these two cultivable mycobacterial agents of human skin disease suggested to me that leprosy bacilli might also grow in this environment.” (Shepard)
Charles Shepard
He had started his experiments in 1957 with M leprae from the nasal washings of leprosy patients and later also from bacilli collected from skin biopsy specimens. He counted the acid-fast bacilli present in a strip across the diameter of the circle and calculated the number of organisms in the original suspension. He then diluted the suspension and injected it into each right hind foot-pad of 20 mice. The lesions that resulted from inoculation of M. leprae could be seen only under the microscope. This achievement would make it possible to test drugs, study immunity, and even investigate the possibility of a vaccine. Professor Michel Lechat has subsequently commented:
What is most probably the third major event in the modern history of leprosy occurred in 1960, when Shepard demonstrated that M leprae recovered from skin biopsy specimens could successfully be grown in the footpads of mice. This brilliant achievement – eagerly awaited since the identification of M leprae almost one century earlier – opened the way to a new area of research in leprosy. From this point on, it became possible to test the sensitivity, or resistance, of M leprae to existing drugs, and to screen new therapeutic compounds for activity against the organism. It was also possible to determine the minimal inhibitory concentration of supposedly effective drugs in the blood of mice.” (WHO) *5
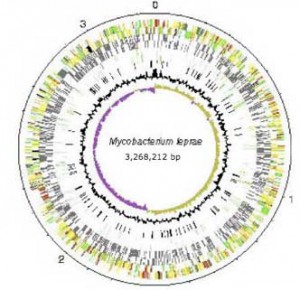
Then the genome of M. Leprae was mapped.
M. leprae can now be conceptualised as a series of genes that can be grouped and described, often by analogy with those identified in another genome, such as M tuberculosis. Technologies other than the microscope are available to view it. Instead of a sample of tissue in serum under a microscope, it now also exists as a genome database that can be explored via MycoBrowser, a genome browser located on the web at http://mycobrowser.epfl.ch/leprosy.html. A search of the genome can be conducted by gene name, region in the genome, gene function, by DNA or protein patterns, by a search of the DNA sequence or protein sequence. Results are presented as a list or a drawing, and the DNA or protein sequence of a single gene can be viewed or downloaded (Jones, 2001, pp. 470-7). The whole sequence of the chromosome is available. Its density, length, number of genes, pseudogenes, and other respective genetic components are enumerated.
Firstly, it is possible to describe something of the evolutionary changes that have taken place. M. leprae has undergone a loss of genes and a subsequent loss of ability to respond to different environments. It is described as a decaying genome: one that has undergone considerable downsizing during its evolution. It has a trajectory and an ancestry – a former self that was more complex. Less than half of the genome contains functional genes. Its “immediate ancestor may have already undergone reductive evolution and … a single clone then expanded and … disseminated globally” (Eiglmeier et al., 2001a, p. 390). Adaptation has been selective and self-interested. Chromosomal rearrangements, gene deletions and duplications have had a profound effect on the biology of M. leprae and in turn on leprosy itself (Cole et al, 2001, p. 459). Yet this decay is evidence of a reduction in redundant functions so that the major repair pathways are still intact (Dawes et al., 2001, p. 411).
 Mapping makes it possible to answer some questions. M. leprae strains from different origins exhibit no obvious, important genome diversity. The genome still retains its full complement of heat shock proteins, explaining why, given its optimal growth temperature is 32°C, it multiplies in the extremities of the body. It is possible to determine the uniqueness of the metabolic pathways of the genome, as well as compare them to that of M. tuberculosis indicating that the survival of M. leprae is dependent on a specialised niche. It has extremely reduced genes for dealing with respiration and an oxygen-rich environment, and hence exists successfully in an intracellular environment, which has relatively constant conditions. The pathogenicity of the mycobacterium depends on its ability to survive in the macrophage or in the Schwann cell. As such it is characterised as “extremely specialised” and it is “irreversibly committed … to a lifestyle characterised by slow growth and necessarily slow central metabolism”. The basis for resistance to dapsone and rifampicin is able to be understood. In addition, the susceptibility of M. leprae to other drugs can be determined. *3
Mapping makes it possible to answer some questions. M. leprae strains from different origins exhibit no obvious, important genome diversity. The genome still retains its full complement of heat shock proteins, explaining why, given its optimal growth temperature is 32°C, it multiplies in the extremities of the body. It is possible to determine the uniqueness of the metabolic pathways of the genome, as well as compare them to that of M. tuberculosis indicating that the survival of M. leprae is dependent on a specialised niche. It has extremely reduced genes for dealing with respiration and an oxygen-rich environment, and hence exists successfully in an intracellular environment, which has relatively constant conditions. The pathogenicity of the mycobacterium depends on its ability to survive in the macrophage or in the Schwann cell. As such it is characterised as “extremely specialised” and it is “irreversibly committed … to a lifestyle characterised by slow growth and necessarily slow central metabolism”. The basis for resistance to dapsone and rifampicin is able to be understood. In addition, the susceptibility of M. leprae to other drugs can be determined. *3
Notes
*1 http://www.who.int/lep/leprosy/en/
*2 They gather together a litany of names: “Lepra Arabum, Elephantiasis Graecorum, Leprosy of the English, Spedalskhed of the Norwegians; Aussatz, Maltzey (of the Middle Ages), Limafalsk (Iceland), Malum mortuum, Malmorte (Salernitan school), Mal rouge (de Cayenne), Mal rosso, juzam (Arab.) Krimskaia, Lepra taurica, Rosa asturiensis, Kushta (India), Fa-fung (China), Koban (Africa), Kokobay (West Indies), Ngerengere and Tuwhenna (New Zealand) Morbus Phoenicius, Morbus herculeus, Satyriasis, Leontiasis (of the old Greeks), Zaraath (Hebrew), Morphoea, Spiloplaxia, Tyria &c., &c” (118).
*3 Adapted from Jo Robertson, In a State of Corruption: Loathsome Disease and the Body Politic (unpublished dissertation, U Qld, 1999)
* 4 Adapted from Jo Robertson, Leprosy and the elusive M. leprae: Colonial and Imperial Medical Exchanges in the Nineteenth Century, Hist Cienc Saude Manguinhos. 2003;10 (Suppl 1):13-40.
http://www.scielo.br/scielo.php?pid=S0104-59702003000400002&script=sci_arttext
*5 Adapted from Jo Robertson, The International History of Leprosy (in preparation for publication)
Sources
Ferdinand Hebra and Moriz Kaposi, On the Diseases of the Skin Including the Exanthemata, ed. and trans. Waren Tay (London: The New Sydenham Society, 1875) 119.
D C Danielssen and C M Boeck, Traite de la Spedalskhed ou Elephantiasis de Grecs (Bergen: D Bayer, 1847).
Charles C Shepard, “Acid-Fast Bacilli in Nasal Excretions in Leprosy and Results of Inoculation of Mice,” American Journal of Hygiene 71 (1960): 147-157 and “The Experimental Disease that Follows the Injection of Human Leprosy Bacilli into Foot-Pads of Mice,” Journal of Experimental Medicine 112 (1960): 445-54.
——, “Multiplication of Mycobacterium Leprae in the Footpad of the Mouse,” IJL 30.3 (1962): 291-306.
WHO, Multidrug Therapy Against Leprosy: Development and Implementation Over the Past 25 Years, 4 (WHO: Geneva, 2004) WHO/CDS/CPE/CEE/2004.46.
